Introduction
Root canal therapy is a dental procedure designed to save a tooth that has been severely infected or damaged from the inside. Rather than removing the entire tooth, this treatment focuses on eliminating the infected tissue from within it, preserving its natural structure and function.
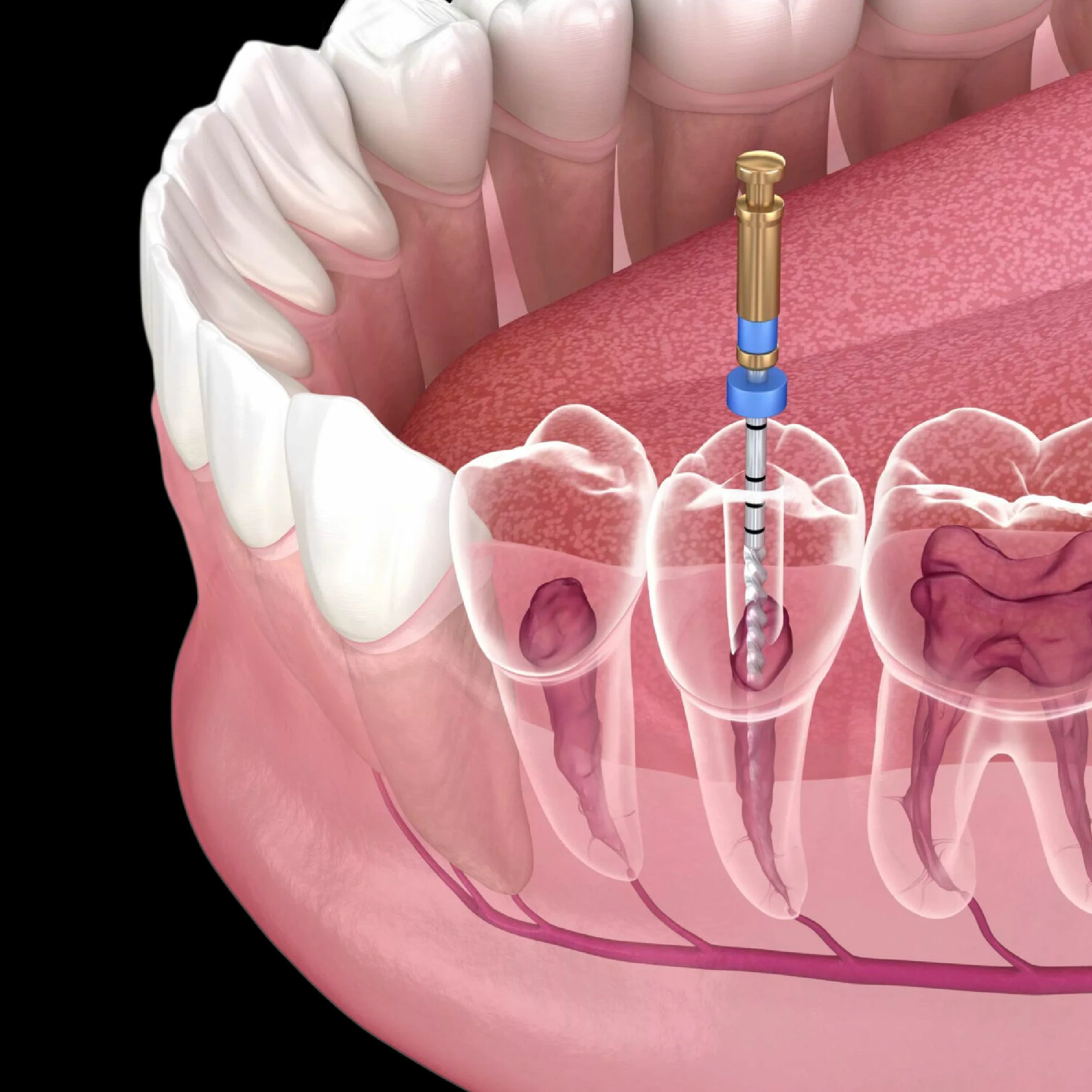
Inside every tooth, there are narrow, hollow spaces known as root canals. These canals extend from the visible part of the tooth, the crown, all the way down to the roots, anchoring the tooth into the jawbone. Depending on the type of tooth, there may be one to four of these canals. Within them lies the pulp, a soft, living tissue made up of nerves, blood vessels, and connective fibers. The pulp plays a vital role during tooth development by supplying nutrients and sensation, but once the tooth is fully matured, it can function even without it.
When the pulp becomes infected due to deep decay, cracks, or trauma, it can cause significant pain and may lead to an abscess if not treated, so know how to relieve severe dental pain. A root canal therapy(also known as endodontic therapy) removes this infected or dead pulp tissue. The dentist or endodontist, a specialist in root canal therapy, carefully cleans and disinfects each canal, then shapes them to prepare for sealing. Once cleaned, the canals are filled with a biocompatible material to prevent bacteria from re-entering and causing further infection.
After the root canal therapy is complete, the tooth is restored with a filling or a crown to strengthen it and restore its full function and appearance. With proper care, a tooth that has undergone root canal therapy can last for many years, functioning just like a natural, healthy tooth.
What Are the Benefits of Root Canal Therapy?
Root canal therapy offers several important benefits for both your oral health and overall well-being. Its primary purpose is to save a natural tooth that has become infected or badly damaged, preventing the need for extraction and more complex restorative procedures. By preserving your original tooth, this treatment helps maintain your natural bite, chewing efficiency, and smile aesthetics, all of which contribute to your long-term dental health.
When the pulp tissue inside your tooth becomes infected or inflamed, often due to deep tooth decay, a dental injury, a crack or fracture, or repeated dental procedures on the same tooth the infection can spread and cause severe pain or even an abscess, so how to relieve severe dental pain. A root canal therapy directly targets the source of the problem by removing the infected pulp, thoroughly cleaning and disinfecting the inside of the tooth, and then sealing the canals to prevent bacteria from returning.
Unlike antibiotics, which can only provide temporary relief, root canal therapy actually eliminates the infection at its root, offering a long-term solution. By treating the problem at its source, the procedure not only relieves pain but also prevents the infection from spreading to surrounding tissues, teeth, or bone.
Once the tooth has healed, your pain and sensitivity should disappear, and you’ll be able to chew comfortably again. Additionally, because the tooth is preserved and restored with a filling or crown, it continues to function naturally and helps prevent other dental issues that might arise from missing teeth, such as shifting, bone loss, or bite misalignment.
In short, root canal therapy is a safe and effective way to:
- Save your natural tooth and avoid extraction.
- Stop the spread of infection and protect neighboring teeth.
- Relieve pain and restore normal chewing and speaking ability.
- Preserve your smile’s natural appearance and structure.
- Provide a long-lasting solution for teeth affected by deep decay or trauma.
With proper care and regular dental checkups, a tooth treated with a root canal therapy can last a lifetime.
What are the signs you need a root canal?
A root canal infection can develop gradually, and in some cases, you might not notice symptoms right away. However, as the infection progresses, the signs you need a root canal usually become more noticeable and uncomfortable. Recognizing these early warning signals can help you seek dental health before the problem worsens.
Common symptoms of a root canal infection include:
- Persistent toothache or sensitivity: This is often the first sign. The pain may feel dull and throbbing or sharp and intense, especially when you bite or chew.
- Sensitivity to hot or cold: You may feel lingering discomfort when consuming hot drinks, cold food, or even when breathing in cool air.
- A pimple-like bump on the gums: Sometimes called a dental abscess or fistula, this bump indicates that pus is forming around the infected tooth as your body tries to fight the infection.
- Swelling around the tooth or jaw: The area may appear puffy or tender to the touch, and in some cases, your face may look slightly swollen.
- Darkened tooth color: The tooth may gradually turn gray or brown as the internal tissue breaks down.
- Bad taste or odor in the mouth: Pus or bacterial buildup inside the tooth can cause a foul taste or smell that doesn’t go away with brushing.
If you experience severe or persistent pain, noticeable swelling, or a sudden change in tooth color, you should know how to relieve severe dental pain and schedule an urgent appointment with your dentist. Ignoring the symptoms can allow the infection to spread deeper into the jawbone or surrounding teeth, making treatment more complicated.
signs you need a root canal
Sometimes, an infected tooth doesn’t cause obvious symptoms at first. However, as the infection worsens, you may begin to experience several telltale signs you need a root canal:
- A recurring pimple or boil on the gums, which may release pus or fluid.
- Swelling of the jaw or cheek, caused by trapped infection inside the bone.
- A tooth that appears darker or discolored compared to the surrounding teeth.
- A loose tooth, as infection can weaken the bone supporting it.
- Pain that radiates to nearby teeth, your jaw, or even your face.
- Discomfort when chewing or pressing on the tooth, making it difficult to eat normally.
- Tender or swollen gums around the affected tooth.
If you notice one or more of these symptoms, don’t delay seeking treatment. A root canal procedure can relieve your pain, stop the infection from spreading, and most importantly, save your natural tooth. Your dentist will perform an examination and may take X-rays to confirm whether a root canal is the right treatment for your situation.
Getting treated early can mean the difference between keeping your natural tooth and losing it, so it’s always best to act quickly when symptoms appear.
What Does a Root Canal Treatment Involve?
A root canal treatment is usually completed over one or more dental appointments, depending on the extent of the infection and the complexity of the tooth’s structure. The procedure is performed by a dentist or an endodontist (a specialist in treating the inner tissues of teeth) and is carefully designed to eliminate infection, relieve pain, and preserve your natural tooth.
Here’s what typically happens during the procedure:
- Examination and X-rays:
Your dentist begins by taking X-rays of your tooth and the surrounding area. These images help them assess the extent of infection, the number of root canals present, and the shape of each canal. This step ensures precise planning and accurate treatment. - Local Anesthesia:
Before the procedure begins, the area around your tooth is numbed using a local anesthetic, ensuring that you remain comfortable throughout the treatment. Although root canal therapy has a reputation for being painful, modern techniques and anesthetics make it virtually painless. - Isolation of the Tooth:
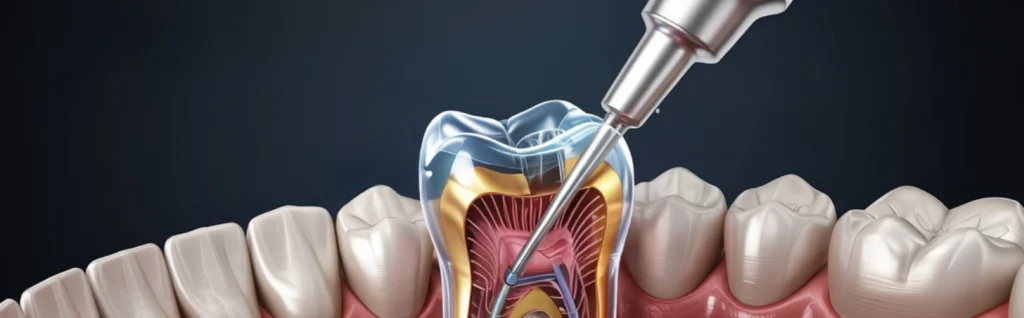
To keep the area sterile and dry, your dentist places a rubber dam and a thin sheet of latex around the affected tooth. This prevents saliva and bacteria from contaminating the site during the procedure. - Accessing the Pulp:
The dentist creates a small opening in the top (crown) of your tooth to access the pulp chamber and root canals. Using fine dental instruments, the infected or dead pulp tissue is carefully removed. - Cleaning, Shaping, and Disinfecting:
Once the pulp is removed, each root canal is meticulously cleaned and shaped to prepare for sealing. The canals are disinfected to remove any lingering bacteria and debris, ensuring the infection does not return. - Temporary Filling (if needed):
If your treatment requires more than one visit, your dentist will place a temporary filling to protect the tooth between sessions and prevent bacteria from entering the canals. - Sealing and Restoration:
Once the canals are completely clean, they are filled with a biocompatible material (usually gutta-percha) to seal them permanently. This prevents reinfection and strengthens the tooth from within.
Finally, the dentist will restore the tooth with either a filling or a crown, depending on the tooth’s condition. The crown adds strength, restores normal function, and protects the treated tooth from further damage.
With proper care, a tooth that has undergone root canal therapy can continue to function normally for many years, often for a lifetime.
References:
https://www.nhs.uk/tests-and-treatments/root-canal-treatment
https://my.clevelandclinic.org/health/treatments/21759-root-canal